
Leena Patil
Department Of Periodontics, Bapuji Dental College and Hospital, Davangere, India.
*Corresponding author: Leena Patil, Department of Periodontics, Bapuji Dental College and Hospital, Davangere, India.
Received: December 02, 2023
Accepted: December 09, 2023
Published: December 15, 2023
Citation: Leena Patil. (2023) “An Overview on Isolated Gingival Recession”. Dental Science and Innovative Research, 1(1); DOI: 10.61148/DSIR/002.
Copyright: Leena Patil. (2023) This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gingival recession is the apical shift in the gingival margin which leads to exposure of the root surface. This may be a static condition or an active process of apical positioning of the gingival margin. 1 Recession may be accompanied by root caries or abraded surfaces, and patients may complain of aesthetic defects or root hypersensitivity. One of the goals of periodontal therapy is to regenerate the lost attachment apparatus of the teeth. Numerous epidemiological studies have demonstrated that gingival recession is most commonly seen in routine practice. Depending on the method of analysis and population involved the prevalence ranges from 40% to 100%. Gingival recession defects can involve single or multiple teeth and can be seen on labial, lingual, and/or interproximal tooth surfaces.2 Based on this it is broadly classified into isolated and multiple gingival recession.
Introduction:
Gingival recession is the apical shift in the gingival margin which leads to exposure of the root surface. This may be a static condition or an active process of apical positioning of the gingival margin. 1 Recession may be accompanied by root caries or abraded surfaces, and patients may complain of aesthetic defects or root hypersensitivity. One of the goals of periodontal therapy is to regenerate the lost attachment apparatus of the teeth. Numerous epidemiological studies have demonstrated that gingival recession is most commonly seen in routine practice. Depending on the method of analysis and population involved the prevalence ranges from 40% to 100%. Gingival recession defects can involve single or multiple teeth and can be seen on labial, lingual, and/or interproximal tooth surfaces.2 Based on this it is broadly classified into isolated and multiple gingival recession.
The exposure of the root surface by the gingival recession is often related to dentine hypersensitivity, root caries, non-carious cervical lesions (NCCLs), compromised plaque control, and unesthetic appearance.3Moreover, the untreated gingival recession inclines, in addition, apical displacement over time, despite good patient motivation.
Therefore, this case report aims to provide a concise and up-to-date overview regarding the etiology, classification, prognosis, and mainly the treatment of isolated gingival recession defects.
Etiology:
A gingival recession occurs due to various causes, it can be seen in cases of normal healthy sulcus without any loss of alveolar bone as well as in pathologic conditions in which alveolar bone is seen.4Conditions due to which alveolar bone loss occurs can be due to anatomical factors or pathological factors.5

Classification: 6
Classification is nothing but categorizing or arranging the condition into various groups according to the established groups. In the field of periodontology, classifications are widely used to categorize defects due to periodontitis according to their etiology, diagnosis, treatment, and prognosis. Thus, the Classification of gingival recession is solely based on diagnosis, prognosis, and treatment planning. Gingival recession can be broadly classified as localized or generalized. For a long time, various classifications for gingival recession have been published starting from:
1. Sullivan Atkin (1968)
2. Mlinek (1973)
3. Liu and Solt (1980)
4. Bengue (1983)
5. Miller (1985)
6. Smith (1990)
7. Nordland and Tarnow (1998)
8. Mahajan (2010)
9. Cairo et al. (2011)
10. Rotundo et al. (2011)
11. Ashish Kumar and Masamatti (2013)
12. Prashant et al. (2014).
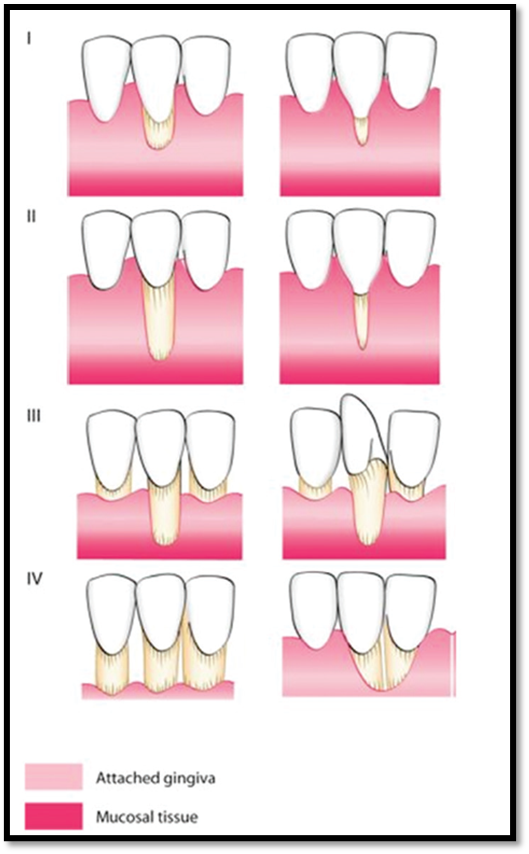
Miller's classification is commonly followed, four types of recession defects were categorized by Miller as follows: 7
• Class I: Marginal tissue recession, which does not extend to the mucogingival junction (MGJ). There is no periodontal (bone or soft tissue) loss in the interdental area and 100% root coverage can be expected.
• Class II: recession of the marginal tissue, which extends to or beyond the MGJ.
• Class III: Marginal tissue recession, which extends to or beyond the MGJ. There is bone or soft tissue loss in the interdental area or there is a malalignment of the teeth, which prevents the attempt at 100% root coverage. Partial root coverage can be expected the amount of root coverage can be determined preoperatively using a periodontal probe.
• Class IV: Marginal tissue recession, which extends to or beyond the MGJ. The bone or soft tissue loss in the interdental area and/or malignment of teeth is so severe that root coverage cannot be expected.
Drawbacks of Miller's classification relate to the uncertain procedures to ascertain the amount of soft-/hard-tissue loss in the interdental area to differentiate Class III and Class IV and the unclear impact of tooth malpositioning. Keeping the outcome in mind Miller's classification is revisited after 35 years, in which the classification of the interdental papilla is added. 8
Type A papilla: There is no interdental bone loss.
The papilla extends 5 mm coronal to the interdental bone crest.
The papilla is ≥3 mm wide at its base at the level of adjacent CEJs.
Complete root coverage is expected.
Type B papilla: There is no interdental bone loss.
The predictability of complete root coverage is compromised.
Type C papilla: There is interdental bone loss, or the tooth is extruded.
If there is interdental bone loss, the papilla may or may not fill the interdental space.
The papilla may be 3 mm wide at its base at the level of adjacent CEJs.
Complete root coverage is not expected but may be achieved under certain circumstances.
Cairo et al. (2011) classified gingival recession based on CAL assessment at buccal and interproximal sites.9
• Recession Type 1:
Gingival recession with no loss of interproximal attachment.
Interproximal CEJ was not clinically detectable in the mesial and distal aspects of the tooth
• Recession Type 2:
Gingival recession associated with loss of interproximal attachment.
The amount of interproximal attachment loss (measured from interproximal CEJ to interproximal pocket depth) was greater than or equal to the loss of buccal attachment (measured from the buccal CEJ to the depth of the buccal pocket).
• Recession Type 3:
Gingival recession associated with loss of interproximal attachment.
The amount of interproximal attachment loss (measured from the interproximal CEJ to the depth of the pocket) was higher than the buccal attachment loss (measured from the buccal CEJ to the depth of the buccal pocket).
Root Coverage Indications: 10,11
• Aesthetic Concern:
Treatment for gingival recession is indicated in several conditions, but of all patient's concern is considered to be the main indication. Patients demand this treatment for esthetic reasons, as excessive exposure of tooth while smiling or communicating can hamper an individual's esthetics.
• Hypersensitivity:
The second most common cause, present in all age range with the majority of cases belonging to the age group of 20-40 years. The prevalence of hypersensitivity is reported to be 3- 57%. In such conditions, patients fail to maintain their oral hygiene, the primary treatment of this being the restorative filling but can be treated in restorative surgical aspect.
• Uneven Gingival Margins:
Uneven or inconsistent gingival margins without any hypersensitivity also pose problems while tooth brushing. This is regularly seen in isolated deep gingival recession cases, as well as in individuals with triangular defects on the buccal side i.e., Stillman's cleft. In such conditions root coverage has to be obtained by surgical approach.
• Root Surface Caries:
Root caries can be observed in young individuals but their prevalence increases as age advances. This can be considered as an indication since it triggers hypersensitivity followed by poor plaque control. Depending upon the possibility to cover the defect with soft tissue along with a restorative procedure treatment can be planned.
• Width of Keratinized Gingiva:
The indication for the treatment of gingival recession may also derive from the inability of brushing at particular sites due to inadequate width or the absence of keratinized tissue.
• Surgical Approach for Isolated Gingival Recession:
The ultimate aim of root coverage with a surgical approach is to achieve an esthetically pleasing appearance, with less amount of probing depth in the healing phase.
Surgical Procedures Used for Root Coverage Can Be Classified as Follows: 12
c) In combination with a barrier membrane
d) In combination with enamel matrix proteins
2) Free soft tissue graft procedures
Pedicle soft tissue graft procedures:
Lateral pedicle flap:
A range of mucogingival surgical approaches can correct gingival recession defects by augmentation of the width and height of keratinized or attached gingiva. It is usually difficult to calculate success achieved in root coverage procedures, as it alters based on multiple factors.
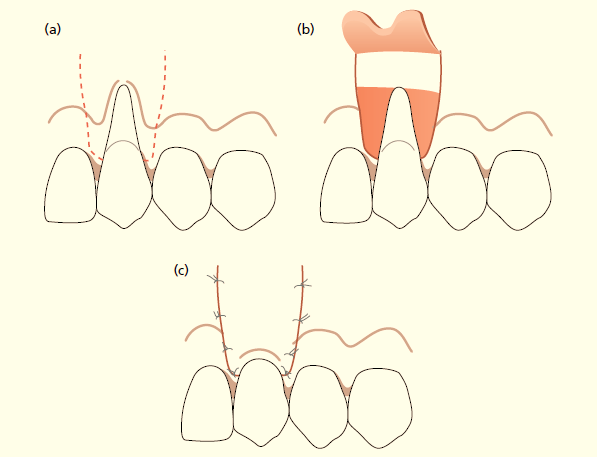
Grupe and Warren et al put forward the concept of laterally sliding flap for the treatment of isolated gingival recession. The existence of good enough width, length, and thickness of keratinized tissue near the vicinity of gingival recession are the indicators of this technique. This technique is appropriate for narrow gingival recessions. The said suggest percent of root coverage with the usage of this technique stages among 34% and 82%. In this technique vertical incisions are given on each side of the defect; the only inflamed area is removed and an incision is extended below the base of the defect. One horizontal incision is given to connect vertical ones. Another incision is placed on the distal side of the defect onto the papilla of the adjacent tooth, carefully taking straight down onto the alveolar mucosa to provide additional mobility to flap. The flap should be wide in dimension to cover the defect. After reflecting the flap, the attached gingiva is dissected from the underlying bone breaking its continuity with alveolar mucosa. Care is to be taken to avoid alveolar bone exposure or tear the thin alveolar mucosa. These all steps leave a freely mobile flap that can be placed onto the defect and sutured.13
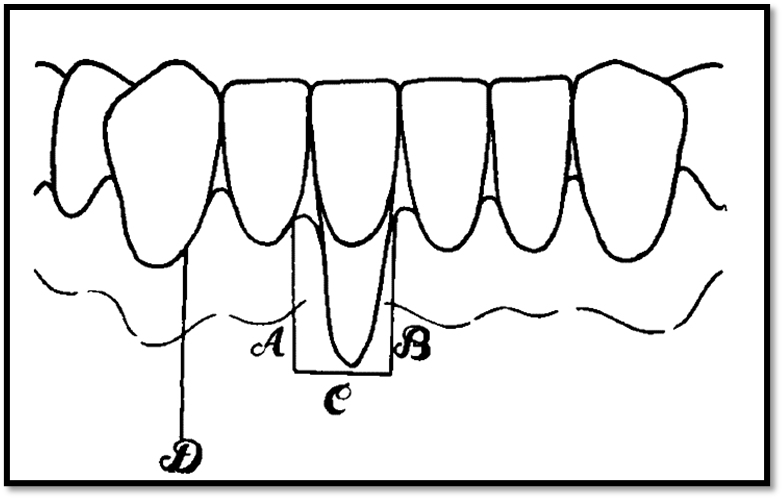
However, there are nevertheless many limitations, which want to be taken into consideration whilst this approach is applied. These include the following:
1. The interdental papillary tissue adjacent to the zone of the recession needs to be thick.
2. There has to be no deep periodontal pocket and bone loss past the mucogingival junction on the interdental regions of the affected tooth.
3. A shallow vestibule also may affect outcomes.
The disadvantages of this technique are viable bone loss and gingival recession on the donor site.14
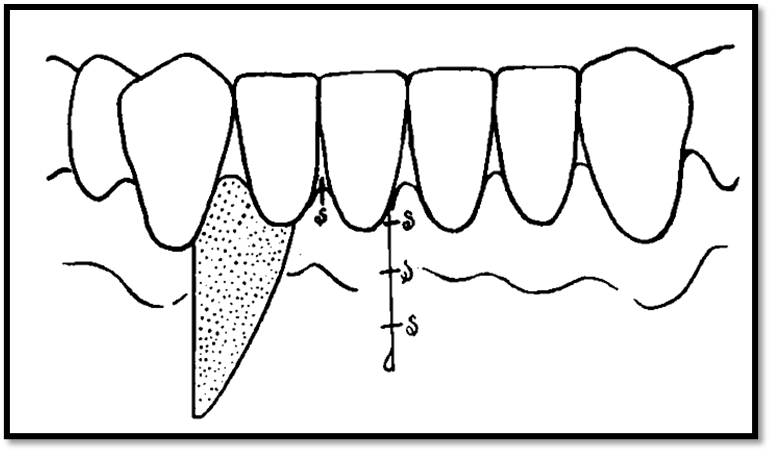
Double Papilla Technique:
In 1968, Cohen and Ross added using the interdental soft tissue to cowl uncovered root surfaces. Subsequently, a double flap of papillae was defined in a partial thickness design, with a CTG by Harris, for the treatment of isolated as well as multiple gingival recession defects.15The double papillae repositioned flap process appears to be pretty beneficial whilst there was the recession of the labial or lingual gingiva, however, destruction of the interdental papillae on either side of the denuded site has no longer occurred. This form of recession is usually seen in individuals practicing incorrect brushing techniques. This pattern of gingival recession is observed at the labial or buccal surfaces of roots in which the concerned tooth is in labial position to the approximating teeth. Prominent muscle attachments or frena can also additionally perpetuate clefts of this type. At times, the clinician has to select the therapeutic technique to restore the lost gingiva. If the adjacent gingival unit is wholesome and the interdental papillae also are healthful, then the therapist ought to pick either the laterally repositioned flap or the double papillae repositioned flap. There are benefits in deciding on the double papillae flap technique over the laterally repositioned flap. One advantage of the double papillae technique is the minimum exposure of underlying periodontium at the interdental donor area.
The wound recovery studies reported that the interdental alveolar bone is much less susceptible to permanent harm after surgical exposure than the labial or buccal plates of bone. The procedure must not bring deformity at the donor site as interdental septa of bone are thicker in comparison to buccal and labial plates. Since the underlying tissues are not exposed much in double papillae flap, the recovery on the donor sites is faster and postoperative sequela are reduced. Another benefit to the double papillae technique is less tension and pull at the repositioned flap, since the flap does now no longer should be pulled from one root floor over to cover another. There additionally appears to be much less risk to embarrass the vascularity in a double papillae flap, considering that every individual papilla has its very own blood supply; whereas, in a laterally repositioned flap, a single pedicle contains the vascular supply for the whole flap. Another benefit in the double papillae approach is abundant gingiva inside the interdental places than at the adjoining labial or buccal surfaces. Since interdental tissue tends to follow the cervical line of the tooth, the zone of attached gingival is commonly more when two papillae are introduced.16
Coronally Advanced Flap:
Taking advantage of the great elasticity of lining mucosa, mucosal flaps can be raised coronally beyond the mucogingival junction to cover denuded root surfaces. Indication for this technique is the presence of a good amount of thickness and height of keratinized tissue at the apex of the denuded root surface. 17
Two types of flap designs: 18
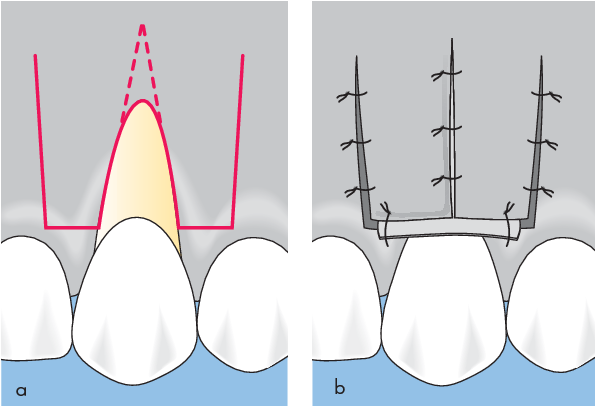
Trapezoidal Flap:
Coronally advanced flap procedure begins with two vertical releasing incisions starting from the point at mesial and distal ling angles just below the CEJ and it ends onto the lining mucosa. Area mesial and distal to recession is prepared for a split-thickness flap and intracrevicular incision is used to connect the flaps. Whereas at the apex full thickness flap is raised to maintain the tissue thickness. A horizontal incision is placed in the periosteum followed by vestibular lining mucosa is bluntly dissected to avoid muscle tension. To release tension from the mucosal flap to advance the blunt coronal dissection, continue to the buccal sides. De-epithelialization of interdental papillae is necessary for the advancement of a flap in a coronal direction. The flap is advanced in such a way that it should be 2-3 mm coronal to the CEJ and sutures are placed, if needed for better wound closure sutures can be given on releasing incisions as well.
The disadvantage of the trapezoidal flap is that the trapezoidal surgical flaps are placed onto the triangular recipient region which leads to an extra amount of soft tissue partly covering the tooth surfaces.
Triangular Flap:
The main advantage of a triangular flap over trapezoidal is a better coverup of the area treated with adjacent soft tissue from an early postsurgical phase. This flap design can be used to treat U shaped or V shaped recession defects. In this flap, design points have to be located precisely around the recession area with the help of orthodontic wire or any such similar device. As the perimeter of U shaped defects are greater releasing incisions are placed less coronally compared to V shaped defect which is narrower with less perimeter. The distinctive feature of this design is that the elevated surgical papillae rotate on the outer side which results in the superimposition of a surgical flap on the recipient bed.
Semilunar Coronally Positioned Flap:
Adequate zone of keratinized tissue is the main selection criteria for this technique. Semilunar incisions are placed above the gingival margin, in case of inadequate keratinized tissue incision can be extended into the alveolar mucosa. The incision has to be extended apically such that the apical end of the incision lies on the bone, and it should terminate laterally on the interdental papilla keeping at least 2mm away from the tip of the papilla to maintain adequate blood supply. A split-thickness flap is elevated coronally with an intra sulcular incision placed in the mid buccal region. In cases of interdental recession tissue from the mid buccal region will be taken coronally or at least till the height of the interdental papilla. If the needed free gingival graft has to be placed at donor site with fenestrations. Advantages of this flap are no tension on the tissues, no vestibular shortening, no loss of interdental papillae. 19


Laterally Moved and Coronally Advanced Flap:
When there is an adequate keratinized tissue apical to the gingival recession coronally advanced flap is considered as the choice of treatment. This technique begins with the horizontal incision at the level of CEJ which is extended at least 3mm, followed by a vertical incision placed parallel to the mesial marginal gingiva. A beveled intrasulcular incision is placed on a distal side of recession extending it up to alveolar mucosa. To move the flap in disto-mesial direction cut back preparation has to be done at the end of the vertical incision to provide great mobility of the flap.
The preparation of the second surgical site and operator dexterities are limiting factors for tissue grafting with the coronally advanced flap technique and accordingly diverse biomaterials/membranes have been proposed in place of genuine tissue grafts. 20
In past decades various barrier membranes are used to increase the connective tissue attachment associated with gingival recession, mean root coverage of 48-87% has been reported with these membranes. 21 A barrier membrane is placed between the surgical flap and root surface to improve healing and prevent interference of gingival epithelial cells and connective tissue in the healing of root coverage. These barrier membranes have shown promising results in terms of root coverage as well as in increased keratinized tissue width. 22
The use of enamel matrix protein derivatives is considered to be one of the successful tissue engineering modalities used for periodontal regeneration. It has been reported that these proteins have a vital role in the formation of cementum during the development of root and periodontal apparatus.
The primary aim of mucogingival surgeries is to obtain excellent pink aesthetics via the restoration of gingival recession. Out of all tissue grafts used, autogenous grafts have shown promising results and are considered as a gold standard. Different types of grafts such as free gingival graft either in de-epithelialized or in partly epithelialized form, subepithelial connective tissue graft, connective tissue graft. 23
Free gingival graft:
This term was first used by Nabers.24Usually obtained from the palate, The hard palate as a donor site for harvesting FGG was first used by Sullivan and Atkins in 1968. It provides stabilization of tissue for a longer time, gives adequate tissue width, keratinization. But, poor blending with adjacent mucosa resulting in poor aesthetics remains the primary concern in this method.23
A subepithelial connective tissue graft:
This autogenous graft is still considered the primary choice in periodontal plastic surgeries. This graft can be gelled with any type of technique such as envelope flaps, double papilla flaps, split-thickness pedicle, etc. Due to abundant blood supply, supreme root coverage and optimal aesthetics are obtained.23 This graft type is advantageous as healing occurs by primary intention at the donor site, improved esthetics are also observed.
Connective tissue graft:
Several disadvantages of other autografts have been overlooked by connective tissue grafts as it creates communication between de-epithelialized connective tissue and recession defect. The pros of using connective tissue grafts are its dual blood supply: one from the recipient bed and the other from the overlying flap, and the perfect blending with adjacent tissues and the best possible aesthetics. 25For the longer existence of graft to provide desirable results graft has to be covered by an overlying flap. This provides adequate blood supply as well nurtures the graft over uncovered root surfaces. 26
Flap design plays a vital role in the success of obtaining optimal root coverage with the connective tissue graft method. Langer and Langer (1985) proposed the placement of vertical releasing incisions, which later on resulted in compromised vascularization followed by scar formation. 27 To overcome these various authors came up with variations on the techniques. Raetzke (1985) proposed An envelope or a pouch flap design eliminating vertical incisions. This technique provided several advantages such as maintenance of optimal blood supply, the better adaptation of graft, and improved postoperative healing as well. Allen (1993) first time combined a connective tissue graft with a tunnel preparation. Such various combinations were tried to achieve desirable outcome.
Conclusion:
The current article reviews the latest knowledge in terms of the etiology, diagnosis, classification, and surgical treatment of isolated gingival recessions. The treatment modality for gingival recession is to be decided based on a detailed valuation of the etiological factors and the degree of involvement of the tissues. In the first-place focus should be given on prevention and then cure of the defect. The extent of gingival recession should be observed for signs of further expansion. In cases of good periodontal health and aesthetically concerned areas, periodontal plastic surgeries are the choice of treatment. Various corrective procedures for recession defects have been anticipated in the periodontal literature and modified with a period based on advanced clinical data. Still for desirable results precise case selection and its management is mandatory.